“Due to a respiratory illness of your dental hygienist—please do not wear perfume or cologne on the day of your appointment. Thank you.” —Sign in my dentist’s office
The potential for allergic reaction is a major concern for the producers of cosmetic products, and extensive work has been done in this field. Respiratory allergy effects can be an important concern regarding fragrance use, but little information is available on this subject. The mechanisms of both reactions are closely related. But exactly how does one determine the respiratory effects of inhaling fragrance? The short answer is: It’s not easy. Something certainly must be measured, and one of those things may well be our old friend IgE (an immunoglobulin that elicits an immune response, explored in the December 2008 “Chemical Reaction” column)—though a host of related signaling molecules are also likely candidates.
The December 2008 “Chemical Reaction” column summarized the recent activities of RIFM and briefly considered the respiratory program, but further attention should be devoted to a recent RIFM paper outlining an approach to the area that was published in 20081. That paper cites TH2-type lymphocyte immune response as a key to respiratory sensitization. It is also suggested that TH1, usually involved in contact sensitization, may have respiratory effects and that there may not be a sharp line between the TH1 and TH2 type response.
It should be remembered that this is part of a broader issue, beyond fragrance, that includes indoor air pollution and environmental atmospheric pollution. The lesson imparted in the paper has broad implications in human health—including the possible connections between dermal and respiratory effects.
Cause and Effect
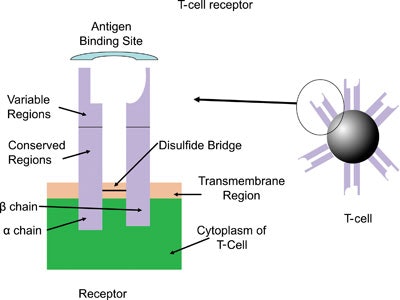
The basic structure of a T-cell is shown in Figure 1. Six receptor binding sites project out of a globular structure. Parts of the chains are the same in all T-cells, while the ends have variable regions that allow for unlimited structural flexibility to respond to any possible allergens.
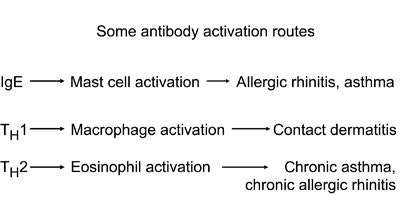
T-helper cells are a sub-group of lymphocytes that play an important role in establishing and maximizing the capabilities of the immune system. Their diversity in function and roles in influencing other cells gives T-helper cells their name. The TH2 type express a number of interleukins (secreted signaling molecules): IL-4, IL-5, IL-10 and IL-11, while TH2 typically express IL-2 and IFN-γ (interferon gamma). A brief view of some pathways triggered by IgE, TH1 and TH2 is shown in Figure 2.
You might think this is a bit involved; indeed it is. In fact, we don’t totally understand all the details of the immune response to allergens from respiratory sensitization. To make it even more complex, there is evidence that respiratory sensitization can be induced by dermal contact with the sensitizer. There is little concrete information in this area. And though it may result only at high levels of exposure, it certainly cannot be ignored in future studies.
Perhaps comparing an allergic reaction to the actions on a battleground would make some of this more intuitive. On the battleground, it is army vs. army; it’s self vs. non-self (invaders) in an allergic reaction. But in both cases, messengers are critical to mobilize forces. In the biological process, IgE is a key messenger for “self,” and quorum sensing2 can sometimes be used to communicate by the invaders. Here, allergens vs. antibodies clash, and when the antibodies win, our bodies repel the allergens. An allergic reaction, then, occurs after the body becomes sensitized to an offending substance. First, the body recognizes an intruder, and plasma cells make large amounts of an antibody to fight the allergen (there is a unique antibody for every type of allergen), and the antibody most commonly associated with allergic reactions is IgE. The IgE antibodies attach themselves to mast cells, which are located in tissue that lines the nose and bronchial tubes. The antibodies stick out from the surface of the mast cells, and the body is now ready for the instance the allergen enters the body. The next exposure causes the antibodies to grab the allergen and send a signal down to the mast cells. A number of chemicals are immediately released, including histamine and heparin. Histamine released in the nose, eyes and sinuses stimulates sneezing, a runny nose and itchy eyes. Released in the lungs, it causes narrowing and swelling of the lining of the airways and the secretion of thick mucus. Released in the skin, it causes rashes and hives.
Determining Respiratory Reactions
Tests to determine respiratory reactions are ongoing considerations. The local lymph node assay (LLNA) may prove useful since respiratory allergens often generate a positive response. While a positive result does not prove a fragrance material is a respiratory allergen, a negative response makes it likely that it is not. Structural alerts may also prove useful, and in silico (computer) models are another option.
While it may seem strange that we don’t know exactly what happens when we inhale fragrances, a few minutes spent looking at the biology involved shows just how great the challenge is to finding the answer. With more than 2,000 chemicals used in fragrances, it will be years before testing protocols are established, data gathered and guidelines issued. We must not overlook the decades of testing on skin that has led to fragrances being as safe as they are now. The expansion of testing into respiration is symbolic of an industry that is second to none in its concern for the consumer.
References
- D Isola et al, Chemical Respiratory Allergy and Occupational Asthma: What Are the Key Areas of Uncertainty? J Appl Toxicol, 28 249–254 (2008)
- S Herman, Talking Germs, GCI, 175 63–64 (2007)
- K Ishizaka, T Ishizaka T, MM Hornbrook, Physico-chemical properties of human reaginic antibody. IV. Presence of a unique immunoglobulin as a carrier of reaginic activity, J Immunol, 97 (1) 75–85 (1966)
Steve Herman is president of Diffusion LLC, a consulting company specializing in regulatory issues, intellectual property, and technology development and transfer. An adjunct professor in the Fairleigh Dickinson University Masters in Cosmetic Science program, his book, Fragrance Applications: A Survival Guide, was published by Allured Business Media in 2001. A former chairman of the SCC’s New York chapter, he was elected to fellow status in 2002.