The subject of SPF (Sun Protection Factor) testing evokes varied responses from the scientific and regulatory communities. Related discussions are provocative, often complex and sometimes exasperating. However, testing cannot be addressed without everyone weighing in, and this includes the testing lab voice and the scientific and regulatory communities.
“[SPF] is obtained by dividing the energy required to produce erythema [sunburn] on product protected fair [Skin types I, II, and III] human skin, by that required to produce erythema on the human subject’s unprotected skin,” explained Dennis Lott, VP technical affairs, Tanning Research Laboratories, manufacturer of Hawaiian Tropic. “Protected skin is that which has received an application of 2 mg/cm2 of SPF product.”
Lott said worldwide test methods expose small areas of the protected and unprotected skin to five to seven increasing doses of ultraviolet (UV) energy produced by an artificial light source called a solar simulator. The first small area on the protected and unprotected skin to exhibit erythema 24 hours after exposure is called the “minimal erythema dose (MEDp)” and MEDu respectively. “An MED is typically defined as an unambiguous redness reaching the borders of the exposure subsite,” said Lott. “The SPF for the individual taking the test is then determined by dividing the amount of energy required to produce erythema on the protected site by that of the unprotected site.” Simply put: SPF = MEDp/MEDu.
The final SPF value is determined by averaging the values obtained from either a 10- or 20-subject panel. “In the United States, a 20-subject panel is used, and the result is statistically massaged in an attempt to determine the point at which 95% of the population will obtain the SPF result,” Lott added.
“Two of the most glaring problems with the SPF test are the fact that the endpoint is not protection, but sunburn, and the fact that only sunburn is measured,” Lott said. “In many individuals, the first reaction to the UV energy may not be erythema but melanogenesis (tanning). For example, subjects frequently show reactions to the UV energy at a lower energy dose than that judged to be erythema.”
Lott said even trained technicians have trouble agreeing on the first unambiguous MED. “It has been reported that technicians’ MED choices vary by as much as 25%, making the resultant SPF vary from lab to lab or from the same lab if judged by different technicians,” said Lott. “Applying a completely uniform film of product over the protected skin site is impossible, and also can cause significant variation in the onset of the first MED. Differences in the solar simulators can produce UV spectra that vary significantly from lab to lab.” He said UV spectra richer in UVA energy compared to UVB energy may tend to make the response from a Type II or III skin type melanogenesis rather than erythema. All these factors cause difficulty in grading subjects’ responses and can produce differences in the final SPF obtained.
Adaptation
Lott said an adaptation can be made that will solve, or at least improve, problems—the pass/fail method. “The basis for the method is simply that no subject response to the UV exposure on the product-protected site is allowed for the sub site to be graded as passing. Thus, the product must truly protect against any UV-induced reaction to pass at a labeled SPF,” said Lott.
The method uses the same parameters as the present SPF method, as well as the same solar simulator, product dosage and number of exposures given to the unprotected site to obtain the MEDu. “The primary difference lies in the UV exposures given to the protected site. The protected site is given four equal doses of UV energy each corresponding to the expected product SPF. Twenty-four hours after exposure, the protected site is examined and each sub site is judged to ‘pass’ if there is no discernible reaction to the UV energy or ‘fail’ if there is any visible reaction, be it melanogenesis or erythema,” said Lott. The test is given to a minimum of five subjects with the goal of obtaining 20 pass or fail values. Based on the values obtained, the product can only pass if, based on binomial statistic tables, the product has at least a 95% chance of being equal to or greater than the tested value.
“The present SPF test is only a measure of erythemal energy that primarily comes from UVB, and the pass/fail test does not differentiate between a response caused by UVB or UVA,” said Lott. “For this reason, it is truly a measure of broad spectrum [UVB and UVA] product protection.” A product that does not have a high amount of UVA protection will not yield as high values with the pass/fail as with the existing SPF methods. “This is important because there is a great deal of worldwide debate today on what UVA test method is to be used, yet almost everyone acknowledges that product users recognize SPF,” continued Lott. “This leads to confusion as to how UVA protection should be labeled to convey the degree of UVA protection yet not detract from the SPF message.”
Lott said advantages of pass/fail include use of fewer human subjects, less potentially harmful UV exposure, endpoint protection, recognition of uneven product application, measurement of UVA and UVB protection, and simple grading.
Key Activities
Joseph Stanfield, president of Sunscreen Research Laboratories, LLC, cited SPF testing approaches worldwide. “The International Method (Cosmetic, Toiletries and Fragrance Association of South Africa; The European Cosmetic, Toiletry and Perfumery Association; Japan Cosmetics Industry Association and the International Sun Protection Factor Test Method and Final Draft October 17, 2002), is by far the most comprehensive and scientifically rigorous method for SPF testing,” said Stanfield. “It includes detailed specifications for solar simulators, detailed instructions for product application and an instrumental method for determining skin types of human volunteers. We can only hope the FDA will adopt the International Method so that rational international harmonization may be achieved.
“Unfortunately, there is no finalized international method for water-resistance testing, and the proposed method is too cumbersome, and actually too lenient, in my opinion,” added Stanfield. “A product can be labeled as ‘very water resistant’ if the SPF, after 80 minutes of water immersion, is above 50% of the static SPF value. Further, the proposed international in vitro method for substantiating UVA protection claims is too complicated and makes incorrect technical assumptions for dealing with products that are unstable or marginally stable in sunlight.”
Achieving agreement is difficult among manufacturers, dermatologists and regulatory agencies. “I am not optimistic that simple, rational methods for substantiating water resistance and supporting UVA protection claims will be achieved in the foreseeable future. This means that confusion among consumers, and even dermatologists, will persist,” added Stanfield.
Key activities of sunscreen formulations include preventing sunburn, reducing UVA dose, providing water resistance and achieving photostability. “This sounds simple, yet there’s no agreement on the recommended SPF level for consumers of varying skin type and outdoor activity, no agreement on the level of UVA protection needed, no test that actually predicts water resistance in actual use and no standard for photostability,” said Stanfield. “I believe SPF numbers are essentially meaningless and water resistance claims misleading. The need for UVA protection has not been studied adequately, and the most often used UVA absorber, avobenzone, is notoriously unstable in sunlight. In fact, I believe it is safe to say that no sunscreen product that contains only avobenzone and octinoxate is photostable.”
Stanfield said sunscreens do work well, and manufacturers would be receiving more complaints and dermatologists would be treating more patients with severe sunburns and skin reactions if they didn’t. Having been involved in SPF testing for 25 years—almost since the U.S. Food and Drug Administration (FDA) published the first proposed Sunscreen Monograph—Stanfield believes it’s time for the industry to address the FDA with clear, scientifically valid information that simplifies testing and protection claims.
“Consumers are confused by multiple SPF numbers, especially the highest numbers that can’t be confirmed by different laboratories,” said Stanfield. “And the ambiguity of UVA and broad spectrum claims and terms such as ‘water resistant’ and ‘very water resistant.’ I believe more effort should go into formulating cosmetically attractive products that consumers find easy to use and don’t have to pay large sums of money for. And I’d like to see new and better sunscreen ingredients and innovation in the science of sun protection.”
FDA Responds
Matthew Holman, interdisciplinary scientist and team leader, FDA, and Susan Cruzan, press office, FDA, say effectiveness testing of over-the-counter (OTC) sunscreen products currently is limited to SPF testing, representing protection against sunburn caused primarily by UVB radiation. “The SPF test has been used in the United States since the 1970s,” said Cruzan. “The FDA has modified it slightly over the past 30 years to incorporate scientific and technical advances and improve accuracy and reproducibility. However, the SPF value on OTC sunscreen products today still represents the same protection measurement that consumers have come to know and understand over the past three decades.
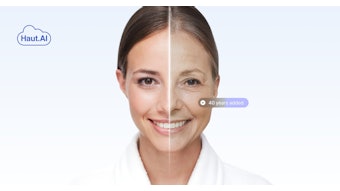
“In the future, the FDA will propose effectiveness testing against UVA radiation,” continued Cruzan. “Scientific studies suggest UVA radiation causes long-term skin damage, such as skin cancer and premature skin aging. Currently, OTC sunscreen manufacturers can test their products for UVA protection by a number of methods published in scientific journals. If an OTC sunscreen product demonstrates effectiveness, then it can be labeled as ‘broad spectrum,’ ‘provides UVA/UVB protection’ or similar claims.”
The FDA is developing a proposal that will require a specific UVA test method and UVA labeling. “After the FDA develops the proposal, we will publish it in the Federal Register, and the public will have the opportunity to comment on it. After reviewing the comments, the FDA will then publish a final rule on UVA testing and labeling. This final rule will have an effective date, after which OTC sunscreen manufacturers will have to comply with the FDA’s UVA testing and labeling,” Cruzan said.
Measurement Approaches
Dieter Kuster, CEO and senior chemist, CA Botana, said in vivo and in vitro testing provide very different measurement approaches. “In vivo testing is less and less common because of total spectrum UVB and UVA, whereby UVA is the longer wavelength and cancer causing, which in most cases shows after several years of consistent exposure to sunlight without protection,” he stated. “Those waves are present from sunrise to sunset, and will penetrate through windows. UVB, the most common wave, is a shorter wave, but will show irritation and, consequently, a burnt condition.” Kuster noted in vitro testing seemed safer, with the sun protection factor determining the amount of protective ingredients used.
“There are organic protectors that, in all cases, destroy free radicals, which are damaging to the cells—(even) more so (to) the Langerhans cells in the skin,” said Kuster. “The inorganic, mineral-derived protection acts more as a reflector of sun rays, and, due to micronization, has become a vital tool for the formulator. Using organic and inorganic protection combined gives you the ultimate sun protection.” Acknowledging the challenge to give the right number for SPF products due to various skin types, geography and mountain or ocean level effects, Kuster suggested classifications such as “Low SPF” (up to 10), “Medium SPF” (11–20) “High SPF” (21–30) and “Extra High” (30 and above) to “take a lot of misinformation out of the SPF game.”
Troubleshooting
Robert Sayre, Ph.D., Rapid Precision Testing Laboratories, cited problems with current sunscreen testing and labeling. “The required standard source only vaguely resembles sunlight. Consequently, the SPF values don’t mean anything in sunlight. The resulting source has too much short wavelength UVB and only half of the UVA in most sunlight. This causes product SPFs to be so unreasonably high as to be meaningless,” Sayre said. “It’s very difficult to get a 15 MED exposure anywhere in a single day, yet products are labeled SPF 30, SPF 45, SPF 65. Most sunscreen ingredients are photounstable, and products fall apart when exposed to sunlight. They don’t seem to work as well in sunlight as in the testing laboratory, and there is no sunlight test for photostability.
“Consequently, high SPFs really don’t mean anything,” Sayre added. “Sunscreen hucksters push high SPFs and UVA protection, yet it’s debatable that any additional UVA protection is needed.” Sayre said that while no one is injured by exposure through window glass, and there are no normal UVA-induced injuries, all experts seem to believe that you must block UVA.Sayre published a paper showing that every sunscreen ingredient tested inhibited the inducible nitric oxide synthase response. This means that some sunscreens act like anti-inflammatory drugs, inhibiting the production of normal sunburn not by blocking UV and preventing injury, but by preventing the response to injury. Further, Sayre suggested too many sunscreen agents are used in too many different products.
Perspectives
David Steinberg, president, Steinberg & Associates, says consumers interpret SPF numbers to mean the amount of time they can stay in the sun and not get burned. A cosmetic chemist will say it’s the ratio of MED with the sunscreen divided by the MED without protection. This means SPF 30 allows you to be exposed to UV radiation for 30 times longer with this product than without sun protection before you get sunburn.
“While these may be true, these are very misleading, and in reality SPF labeling of products is a fraud, as far as I’m concerned,” said Steinberg. “Why? Who knows their MED? It usually is thought to be about 20 minutes in summer sun in the greater New York area. But this varies by different areas, angle of the sun, time of year and more.
“The distortion of SPF as tested as opposed to what is applied has led many to wonder about better alternatives,” said Steinberg. “The distortion is being compounded now with suggested UVA testing. The Japanese PPD (Persistent Pigment Darkening) method for determining amount of UVA protection is a ratio similar to SPF but for UVA, which, unfortunately, calls for the same high amount to be used. It is clear we can’t change SPF test methods to reflect reality. One suggestion is to continue SPF and the number, but have real product category designations of low, medium and high sunburn protection based on what is really applied—like 0.2 milligrams per square centimeter.”
“When all is said and done, we are seeking protection from sunburn. Put your SPF on, but let’s have a new thing called Sunburn Protection, and run an in vivo test using a level that people actually apply,” Steinberg added. “If we could get the world to buy into this—consumers, dermatologists and the medical community—then it will be done and it will start going on labels. Ultimately, you should be allowed to make only two claims: your product is broad spectrum and it protects against UVA/UVB rays.”